Understanding Cushing Syndrome: Causes, Symptoms, Diagnosis, and Latest Advances in Treatment (2025 Update)
Cushing syndrome, a rare but serious medical condition, has been gaining attention in recent years due to advancements in treatment and increased awareness. This condition, caused by prolonged exposure to high levels of cortisol, can significantly impact a person's quality of life if left untreated. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for Cushing syndrome, as well as the latest developments in research and therapies in 2025.
What is Cushing Syndrome?
Cushing syndrome occurs when the body is exposed to excessive levels of cortisol, a hormone produced by the adrenal glands. Cortisol plays a vital role in regulating metabolism, immune response, and stress. However, when cortisol levels remain elevated for an extended period, it can lead to a range of health issues.
Types of Cushing Syndrome
- Exogenous Cushing Syndrome: This is the most common form and is caused by prolonged use of corticosteroid medications, such as prednisone, often prescribed for conditions like asthma, rheumatoid arthritis, or lupus.
- Endogenous Cushing Syndrome: This occurs when the body produces too much cortisol due to:
- Cushing’s Disease: A pituitary tumor secretes excessive adrenocorticotropic hormone (ACTH), which stimulates cortisol production.
- Adrenal Tumors: Benign or malignant tumors in the adrenal glands directly produce cortisol.
- Ectopic ACTH Syndrome: Tumors outside the pituitary gland, such as in the lungs, produce ACTH.
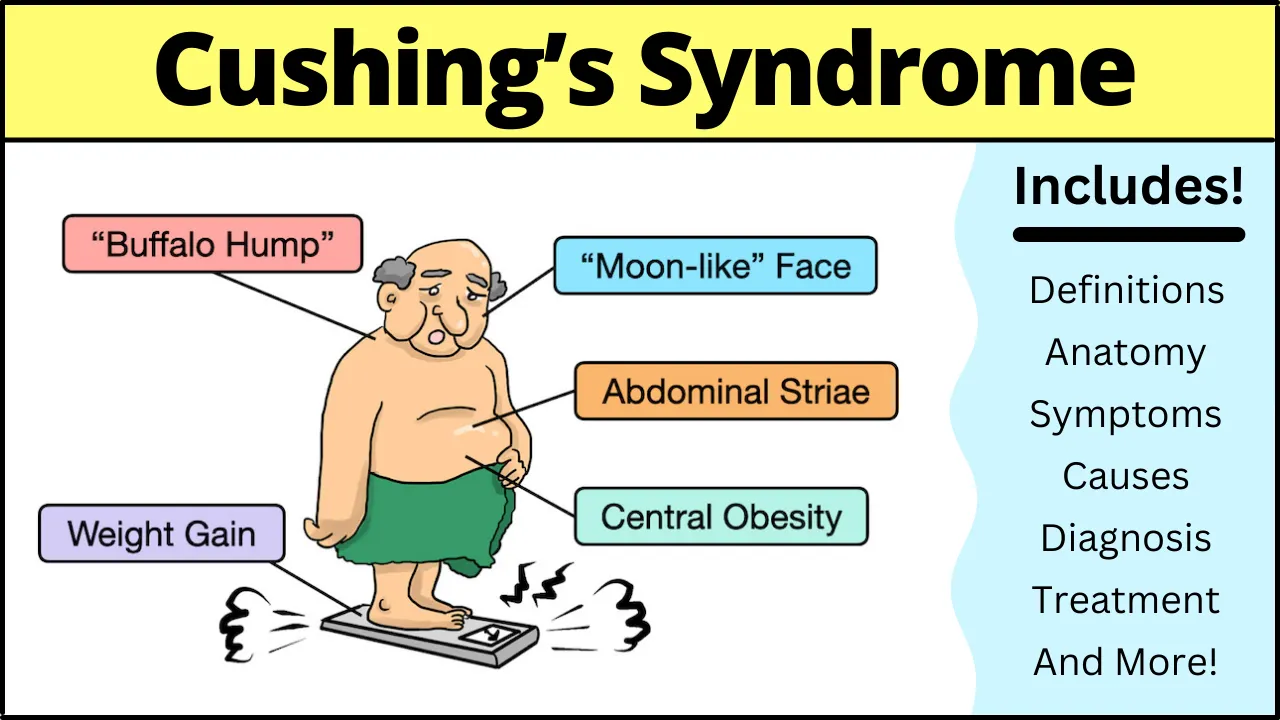
Symptoms of Cushing Syndrome
The symptoms of Cushing syndrome can vary widely depending on the severity and duration of cortisol exposure. Common signs include:
- Physical Changes:
- Weight gain, particularly around the abdomen and face (commonly referred to as "moon face").
- Fat deposits between the shoulders, known as a "buffalo hump."
- Thin skin that bruises easily and slow-healing wounds.
- Purple stretch marks (striae) on the abdomen, thighs, or breasts.
- Muscle and Bone Issues:
- Muscle weakness.
- Osteoporosis, leading to fractures.
- Metabolic and Cardiovascular Problems:
- High blood pressure.
- High blood sugar or diabetes.
- Psychological Symptoms:
- Depression, anxiety, and mood swings.
- Cognitive difficulties, such as memory problems.
- Reproductive and Hormonal Changes:
- Irregular or absent menstrual periods in women.
- Decreased libido and erectile dysfunction in men.
Causes of Cushing Syndrome
The underlying causes of Cushing syndrome depend on whether it is exogenous or endogenous:
- Exogenous Causes:
- Long-term use of corticosteroid medications is the leading cause of Cushing syndrome. These medications are often prescribed for chronic inflammatory or autoimmune conditions.
- Endogenous Causes:
- Pituitary Tumors: These benign tumors, known as adenomas, are the most common cause of endogenous Cushing syndrome.
- Adrenal Tumors: These can be benign (adenomas) or malignant (adrenocortical carcinomas).
- Ectopic ACTH Production: Certain cancers, such as small cell lung cancer, can produce ACTH, leading to excess cortisol.
Diagnosis of Cushing Syndrome
Diagnosing Cushing syndrome can be challenging due to the overlap of symptoms with other conditions like obesity or metabolic syndrome. A thorough evaluation by a healthcare provider is essential. The diagnostic process typically includes:
- Medical History and Physical Examination:
- A detailed review of symptoms, medical history, and medication use.
- Physical examination to identify characteristic signs like moon face or purple stretch marks.
- Laboratory Tests:
- 24-Hour Urine Free Cortisol Test: Measures cortisol levels in urine collected over 24 hours.
- Late-Night Salivary Cortisol Test: Assesses cortisol levels in saliva, which should be low at night.
- Dexamethasone Suppression Test: Evaluates how cortisol levels respond to a synthetic steroid.
- Imaging Studies:
- MRI or CT Scans: Used to identify tumors in the pituitary or adrenal glands.
- Chest X-rays or CT Scans: To detect ectopic ACTH-producing tumors.
- Inferior Petrosal Sinus Sampling (IPSS):
- A specialized test to determine whether excess ACTH is coming from the pituitary gland or another source.
Latest Advances in Cushing Syndrome Treatment (2025)
Treatment for Cushing syndrome aims to reduce cortisol levels and address the underlying cause. Recent advancements in research and therapies have provided new hope for patients.
1. Surgical Options
- Minimally Invasive Surgery: A recent study published in Cushing’s Disease News (January 2025) highlights the effectiveness of partial adrenalectomy, a minimally invasive procedure that removes only the tumor-affected portion of the adrenal gland. This approach preserves adrenal function and reduces the risk of complications.
- Transsphenoidal Surgery: For pituitary tumors, this surgery remains the gold standard. Advances in surgical techniques have improved success rates and reduced recovery times.
2. Medications
- Clofutriben: A promising new drug currently in clinical trials (RESCUE trial) has shown the ability to normalize cortisol levels in patients with endogenous Cushing syndrome. Unlike traditional therapies, clofutriben targets cortisol production within cells, reducing the risk of adrenal insufficiency.
- Relacorilant: Developed by Corcept Therapeutics, this drug is designed to block cortisol’s effects without lowering its levels, offering a safer alternative for long-term management.
- Ketoconazole and Metyrapone: These medications remain standard options for controlling cortisol production.
3. Radiation Therapy
- For patients with pituitary tumors who cannot undergo surgery or whose tumors persist after surgery, radiation therapy is an effective option.
4. Lifestyle and Supportive Care
- Diet and Exercise: Managing weight and maintaining bone health are crucial for patients with Cushing syndrome.
- Mental Health Support: Addressing depression and anxiety through therapy or medication is an integral part of treatment.
Recent Case Studies and Awareness
Amy Schumer’s Diagnosis
In January 2025, comedian Amy Schumer revealed her experience with Cushing syndrome, which was diagnosed after online comments about her swollen face prompted her to seek medical advice. Schumer’s case highlights the importance of public awareness and early diagnosis. She attributed her condition to steroid injections received after surgery, a common cause of exogenous Cushing syndrome.
Pediatric Cases
A recent case study reported in Cushing’s Disease News (January 2025) described a 5-year-old boy who developed Cushing syndrome due to prolonged use of high-potency corticosteroid creams for psoriasis. This underscores the need for caution when using corticosteroids, especially in children.
Risks and Complications of Untreated Cushing Syndrome
If left untreated, Cushing syndrome can lead to severe complications, including:
- Cardiovascular diseases, such as heart attack or stroke.
- Type 2 diabetes.
- Osteoporosis and fractures.
- Infections due to a weakened immune system.
- Psychological issues, including severe depression.
Future Directions in Cushing Syndrome Research
The field of endocrinology is rapidly evolving, and researchers are exploring innovative approaches to treat Cushing syndrome:
- Gene Therapy: Scientists are investigating the potential of gene-editing technologies like CRISPR to target genetic mutations associated with cortisol overproduction.
- Biomarker Discovery: Identifying specific biomarkers could improve early diagnosis and treatment monitoring.
- Patient-Centered Care: Advances in telemedicine and wearable devices are enabling personalized treatment plans and real-time monitoring of cortisol levels.
Conclusion
Cushing syndrome is a complex condition that requires a multidisciplinary approach for effective management. With recent advancements in minimally invasive surgery, novel medications like clofutriben and relacorilant, and increased public awareness, the outlook for patients with Cushing syndrome is improving.
Early diagnosis and treatment are critical to preventing complications and improving quality of life.
As we move forward in 2025, continued research and innovation will undoubtedly bring new hope to those affected by this challenging condition.
If you or someone you know is experiencing symptoms of Cushing syndrome, consult a healthcare professional for a thorough evaluation and personalized treatment plan.